
NEWS
Multiple PADN Case Studies – Nanjing First Hospital Cardiovascular Department
Recent advances in the understanding of pulmonary arterial hypertension (PAH) have led to updates in diagnostic approaches, risk stratification, and treatment strategies. The sympathetic nervous system is recognized as playing an important role in the development and progression of PAH. Since the innovation and clinical application of percutaneous pulmonary artery denervation (PADN) by Professor Shaoliang Chen, increasing clinical evidence has demonstrated its therapeutic potential. As this technique becomes more widely adopted worldwide, interventional therapy has entered a new era as an adjunct to targeted medical therapy for PAH. With growing experience, more complex and challenging cases have been encountered.
Case 1 – First Reported PADN via Internal Jugular Vein Approach
69-year-old woman was admitted with worsening chest tightness and dyspnea over the past week, on a background of similar symptoms for approximately two years. Her medical and surgical history included surgical repair of a ventricular septal defect, atrial fibrillation, and splenectomy. Exertional dyspnea persisted following optimal pharmacotherapy, and she was classified as New York Heart Association (NYHA) functional class III based on evaluation.
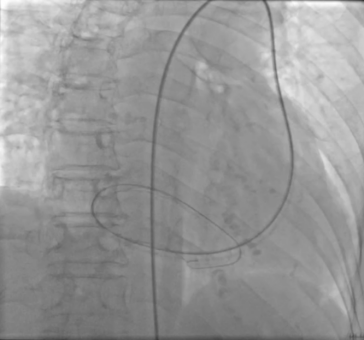
Echocardiography revealed coronary sinus dilation, suggesting a persistent left superior vena cava. Pulmonary computed tomography angiography (CTA) demonstrated an enlarged azygos vein, indicating a possible inferior vena cava (IVC) developmental abnormality.
During right heart catheterization, the guidewire was observed to pass along the left side of the spine through the IVC into the azygos vein, then through the persistent left superior vena cava into the coronary sinus, returning to the right atrium and passing through the tricuspid valve. PADN via the IVC route was not feasible due to the persistent left superior vena cava, which also precluded access via the left subclavian or left internal jugular veins.
Following multidisciplinary discussion, the team elected to perform PADN via the right internal jugular vein — the first such approach reported worldwide. Pre-procedure CTA was used to evaluate pulmonary artery anatomy and select an appropriate ablation catheter. Via the right internal jugular vein, the catheter was advanced across the tricuspid valve, through the right ventricle, and into the pulmonary artery. Target ablation points were identified, and ablation was successfully performed.

Clinical Outcome:
Post-procedure, mean pulmonary artery pressure (mPAP) decreased from 26 mmHg to 21 mmHg, pulmonary capillary wedge pressure (PCWP) decreased from 16 mmHg to 13 mmHg, CO increased from 4.4 L/min to 6.1 L/min, and PVR decreased from 2.27 Wood units to 1.31 Wood units. The patient tolerated the procedure well and reported significant relief of dyspnea postoperatively.

Case 2 – PADN in Severe Pulmonary Artery Aneurysmal Dilatation
A 37-year-old man from Shaanxi Province was admitted to the hospital with uncontrolled pulmonary arterial hypertension (PAH). He had a history of surgical repair for ventricular septal defect 25 years earlier and developed PAH symptoms eight years ago. He had been on long-term triple therapy without symptom relief and continued to experience persistent chest tightness, dyspnea, marked ascites requiring long-term drainage, facial cyanosis, and was bedridden.
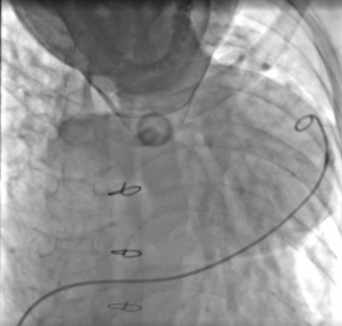
Pulmonary CTA revealed aneurysmal dilatation of the main pulmonary artery, with a maximal diameter of 99 mm — the largest recorded in China. Potential concerns included variations in sympathetic nerve distribution, inadequate catheter contact, risk of PAH crisis, or pulmonary artery aneurysm rupture. A detailed procedural plan and emergency contingency measures were prepared. Ablation was performed at multiple points at the junction of the main pulmonary artery and the ostium of the left pulmonary artery.
Clinical Outcome:
Pulmonary artery systolic pressure decreased from 131 mmHg to 119 mmHg, mPAP decreased from 70 mmHg to 62 mmHg, CO increased from 4.19 L/min to 4.8 L/min, and PVR decreased from 11.9 Wood units to 10 Wood units. The patient reported marked symptomatic relief, and postoperative imaging showed significant reduction in ascites and pericardial effusion. The patient was discharged on postoperative day 3.
Case 3 – PADN in the Oldest Reported Patient
A 98-year-old woman from San Francisco, USA, was admitted to the hospital with chest tightness and dyspnea for five months. Echocardiography showed an ejection fraction (EF) of 66%, left atrial enlargement, moderate mitral regurgitation, and severe pulmonary hypertension (estimated systolic pulmonary artery pressure of 71 mmHg). Right heart catheterization revealed a mean pulmonary artery pressure (mPAP) of 46 mmHg and a pulmonary capillary wedge pressure (PCWP) of 22 mmHg, consistent with a diagnosis of group 2 pulmonary hypertension (PH) due to left heart disease. Given her use of dapagliflozin and diuretics, the presence of elevated pulmonary vascular resistance (PVR) of 4.9 Wood units, and the limited treatment options for heart failure with preserved ejection fraction (HFpEF), the team proposed that PADN could be beneficial. The patient and her family expressed strong interest in PADN after learning of its efficacy in left heart disease-associated PH.
Clinical Outcome:
mPAP decreased from 46 mmHg to 43 mmHg, PCWP from 22 mmHg to 20 mmHg, CO increased from 4.9 L/min to 5.8 L/min, and PVR decreased from 4.9 Wood units to 3.9 Wood units. The procedure was completed without complications, and the patient recovered well. This is the oldest PADN patient reported to date.


Pulmonary Artery Stent Implantation in a 37-Year-Old Female with Pulmonary Artery Stenosis
A 37-year-old woman was admitted to the hospital with chest tightness and dyspnea. She had been diagnosed with right pulmonary artery stenosis and had previously undergone two pulmonary artery balloon dilatation procedures without symptomatic improvement, remaining severely exercise-intolerant.
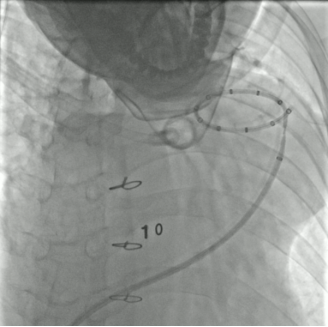
She was evaluated by Professor Hang Zhang at Nanjing First Hospital and diagnosed with pulmonary artery stenosis secondary to pulmonary arteritis, consistent with World Health Organization (WHO) group 4 pulmonary hypertension. After comprehensive assessment, pulmonary artery stent implantation was proposed and performed by Professor Zhang and Director Zhiming Wu. Pulmonary angiography and intravascular ultrasound (IVUS) demonstrated a minimal luminal diameter of 4.5 mm at the stenotic site. A 12 mm × 30 mm stent was selected and precisely deployed at the lesion site.
Post-procedure, mean pulmonary artery pressure decreased from 42 mmHg to 30 mmHg, and the translesional pressure gradient decreased from 67 mmHg to 20 mmHg. The patient reported significant symptomatic improvement.



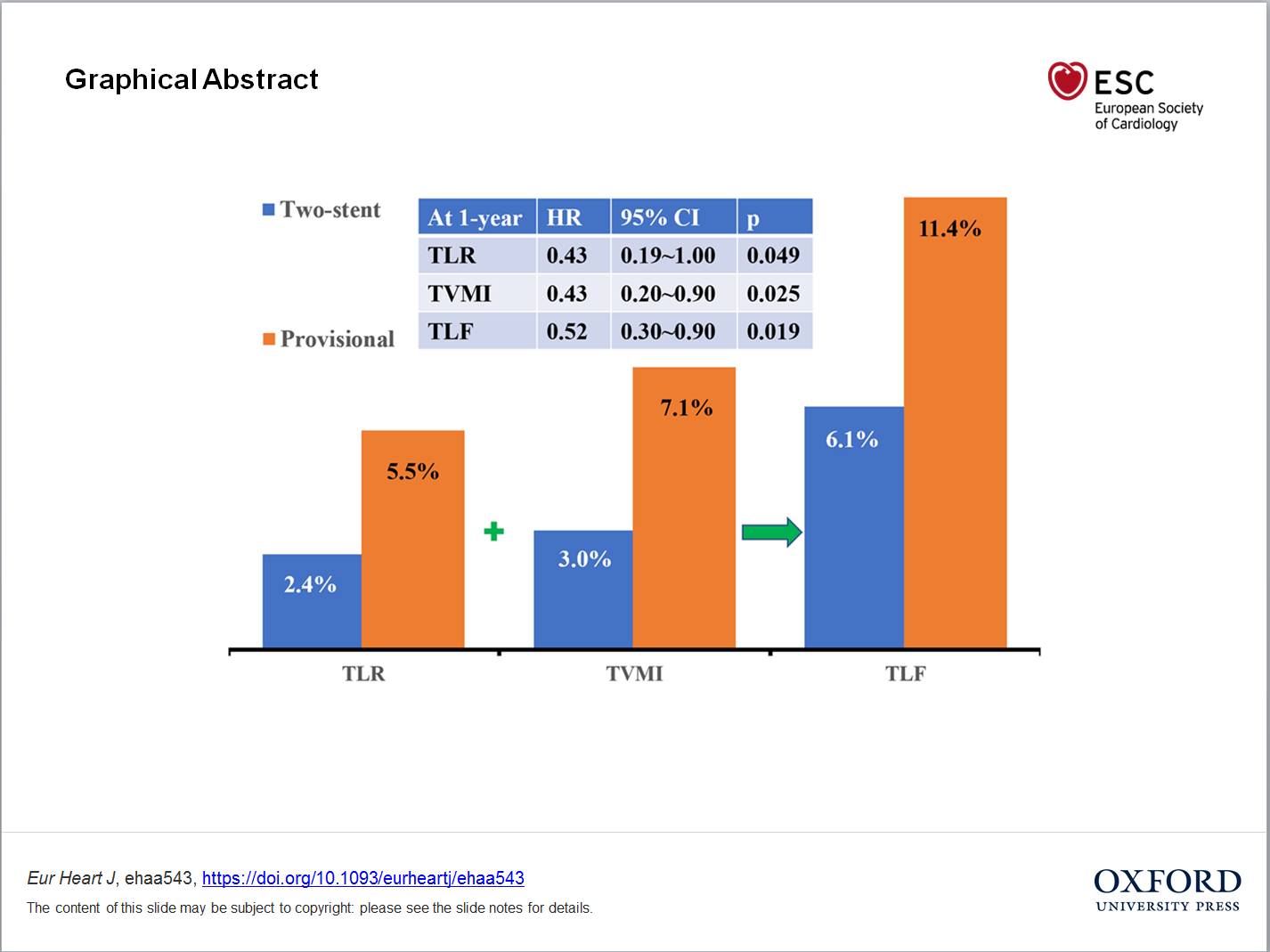
DEFINITON Trial Released by EuroPCR 2020
Multicentre, Randomized Trial Comfirms Two-stent Approach Improves Clinical Outcomes Compared with Pro...

SCAI 2020 - Invitation to Scientific Sessions
The Intersection of Innovation and Practice.

Introduction to the Department of Cardiology in Nanjing ...
On April 1, 2020, the introduction about Department of Cardiology of Nanjing First Hospital as "Cardiac Centre...

CSC-SHC-NHAM Anti-Pandemic Conference Webinar...

Nanjing First Hospital & Sarawak Heart Centre
The Belt and Road Partenership